Tuesday, January 25
“Reducing racial and ethnic disparities in health outcomes is more difficult than simply standardizing the care provided to patients... Eliminating disparities requires truly patient-centered care—that is, individualized care by clinicians who appreciate that patients’ beliefs, behaviors, social and economic challenges, and environments influence their health outcomes.” - Marshall Chin
|
You may have heard about the wealth gap, but have you heard about the wealth-health gap?
Both institutional racism and differences in socioeconomic status lead to disparities across living conditions, limit access to quality health care, and contribute to chronic stress. For example, in a summary of several studies, the American Bar Association notes that "the poverty in which Black people disproportionately live cannot account for the fact that Black people are sicker and have shorter life spans than their white complements...racial and ethnic minorities receive lower-quality health care than white people - even when insurance status, income, age, and severity of conditions are comparable."
These factors lead to shorter life spans and higher likelihood of adverse health outcomes for people living in poverty and BIPOC (Black, indigenous, and people of color) populations. Healthcare costs also make up a significant portion of a household’s annual budget, placing additional stress on families that may or may not have insurance and access to quality care.
In addition, some communities, such as Black Americans, are much less likely to trust their healthcare providers and healthcare institutions. The Tuskegee Syphilis Study is one of the most egregious demonstrations of the origins of such distrust.
The COVID-19 pandemic has shed new light on the inequities in our healthcare system.
“We know viruses do not discriminate based on location, race, ethnicity, or national origin,” says Jimena Loveluck, Health Officer for Washtenaw County, Michigan. “However, viruses like COVID-19 can highlight health disparities that are deeply rooted in our society.”
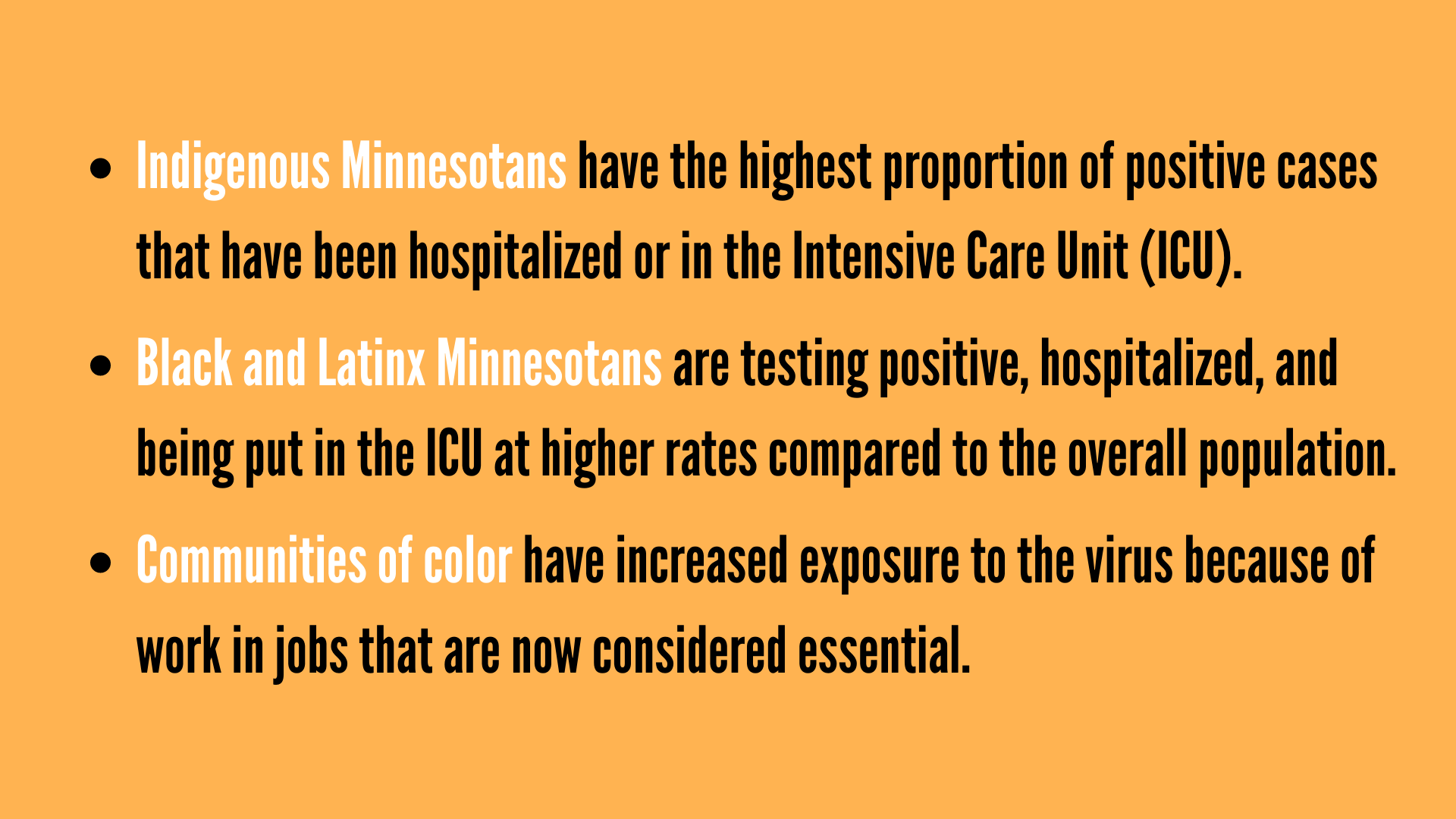
In Minnesota, a disproportionate number of total confirmed COVID-19 cases and deaths have occurred in BIPOC patients.
When looking at Minnesota's COVID-19 data by race and ethnicity, you can see how the existing gap in healthcare continues to become exacerbated:
Did you know?
- Black women are two times more likely to experience a stillbirth than their white counterparts (One Economy, 2020)
- Adults of color, women, and low-income individuals report higher rates of childhood trauma compared to other groups (Iowa ACEs 360, 2020)
- Only 1 in 3 Black Americans who needs mental health care receives it (American Psychiatric Association, 2017)
- 34% of Black trans and nonbinary individuals have had one or more negative experiences with a healthcare provider in the last year (National Center for Transgender Equality, 2015)
Today’s Challenge: Do one or more of the following…
OPTION 1: Hear Dr. Camara Phyllis Jones explain social determinants of health through her analogy of the “cliff of good health” (5:18), in a video collaboration with the Urban Institute.
OPTION 2: Watch David. R Williams, a public health sociologist, on the TED stage (17:19) discuss why race and deep-rooted systemic racism have such a profound impact on health.
OPTION 3: Check out this Fact Sheet from the American Psychological Association exploring the compounding impact of socioeconomic status and race on health.
OPTION 4: Hear the story of Henrietta Lacks (6:36), an African American woman whose cells have been used to test the effects of radiation and poisons, to study the human genome, to learn more about how viruses work, and played a crucial role in the development of the polio vaccine. It is most important to note that, while Ms. Lacks’s have been the source of life-saving medical solutions, no consent was obtained to culture her cells, nor were she or her family compensated for their extraction or use.
OPTION 5: Published in the journal Nature, a recent study found that millions of Black people have been affected by racial bias in health-care algorithms used by many U.S. hospitals, resulting in Black people being less likely to be referred to programs than white people who were equally sick.
OPTION 6: A research team at Mayo Clinic developed a measurement called HOUSES, which looks at socioeconomic status to understand health disparities and outcomes. Socioeconomic standing particularly amplifies the disparities between non-Hispanic white community members and community members of color.
|
.png)
.png)